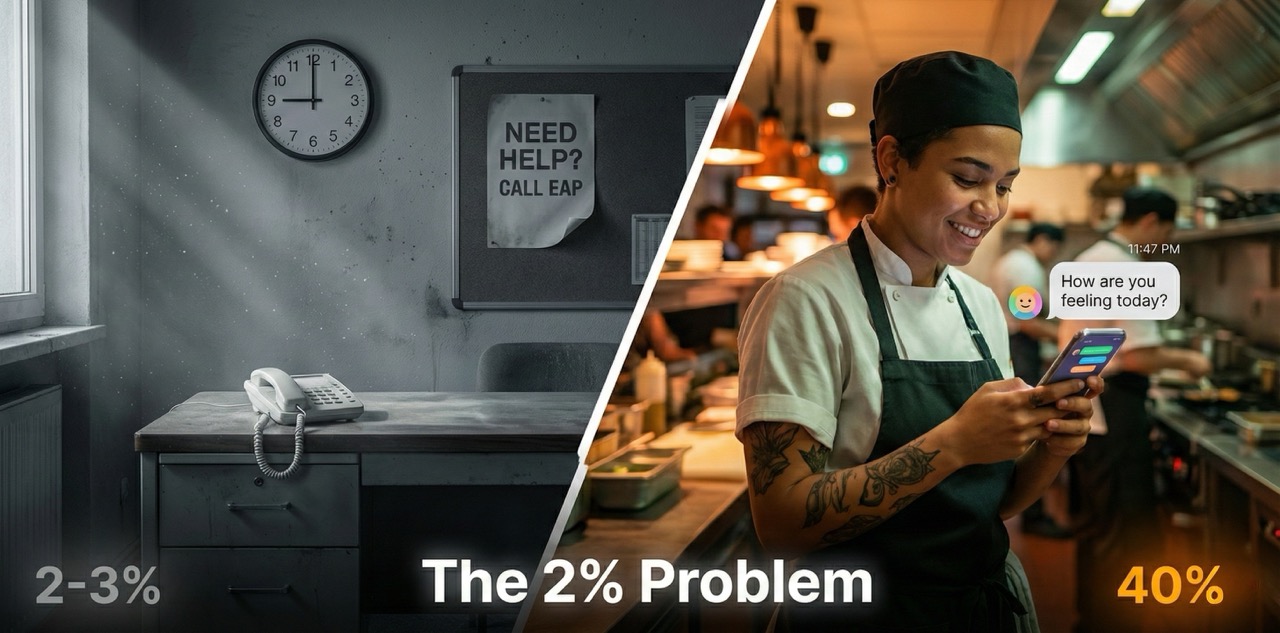
Here's a number that should concern every QSR operator in Australia: 2-3%.
That's the typical EAP utilisation rate in hospitality, retail, and manufacturing (Sonder).
You're paying for a mental health support service. It's in your onboarding pack. It's on a poster in the break room. And 97% of your workforce will never touch it.
Meanwhile, 61% of hospitality workers reported experiencing a mental health condition in the past 12 months – nearly three times the general population rate of 21.5% (Healthy Workplaces SA; Australian Bureau of Statistics).
Something is badly broken here. And understanding why is the first step to fixing it.
The Scale of What We're Dealing With
Let's be clear about the numbers.
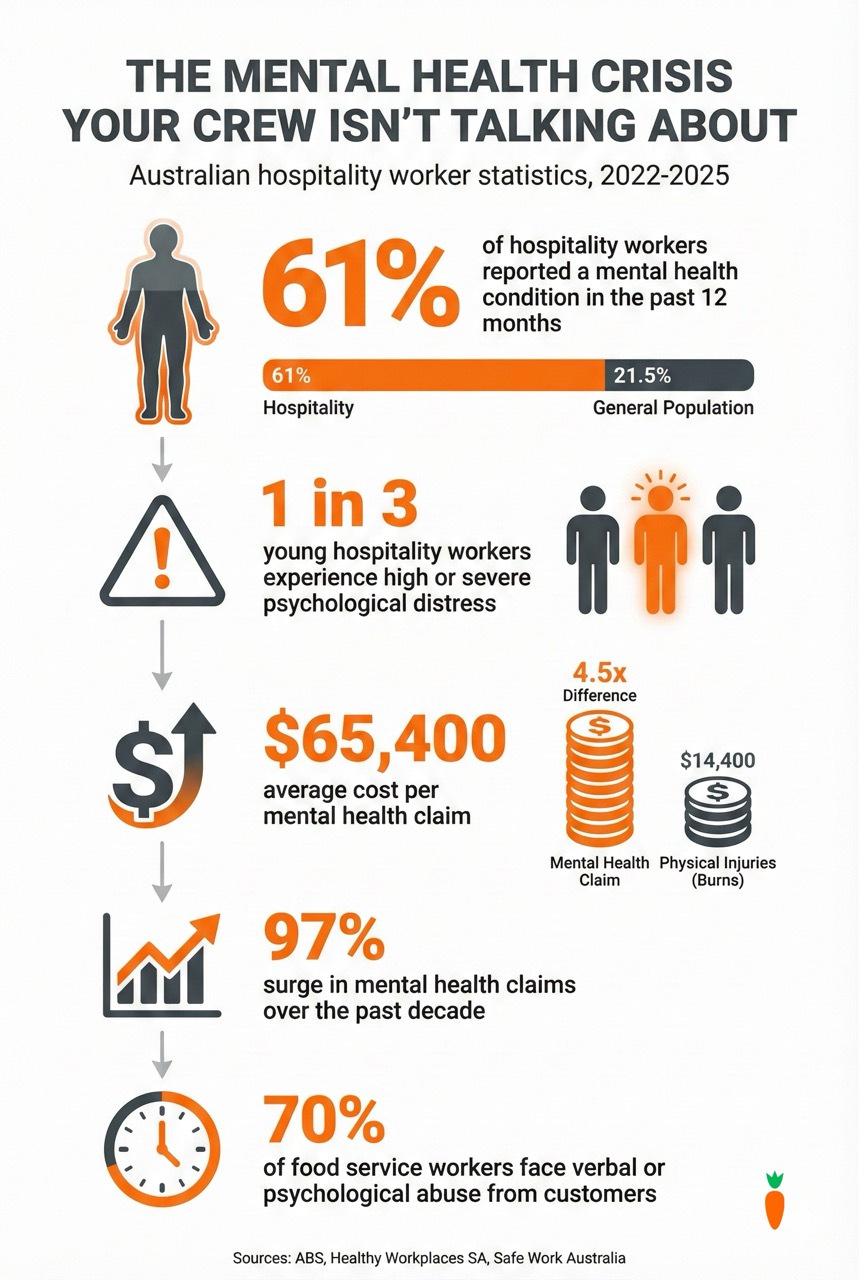
The accommodation and food services sector has seen a 97% surge in mental health claims over the past decade, now representing 10.5-12% of all serious workers' compensation claims nationwide (Scratchie industry analysis). In 2023-24, that translated to approximately 14,600-17,600 claims across Australia.
The cost? An average of $65,400 per mental health claim – more than four times the cost of physical injuries like burns at $14,400 (Scratchie industry analysis).
Young workers are hit hardest. Among Australians aged 16-24, 38.8% have a 12-month mental disorder – and that's the general population (Australian Bureau of Statistics). In hospitality, with its irregular hours, customer abuse, and "push through" culture, the rates are significantly higher.
Research from The Burnt Chef Project indicates one in five hospitality professionals experience depression, while an Australian study found chefs were significantly more likely than the general population to die by suicide (ABC News, 2024).
This isn't just a welfare issue. It's a business crisis hiding in your workers' compensation data.
Why Traditional EAPs Fail Your Crew
So why does a support service that's available to everyone get used by almost no one?
The answer lies in a fundamental mismatch between how traditional EAPs work and how young hospitality workers actually live.
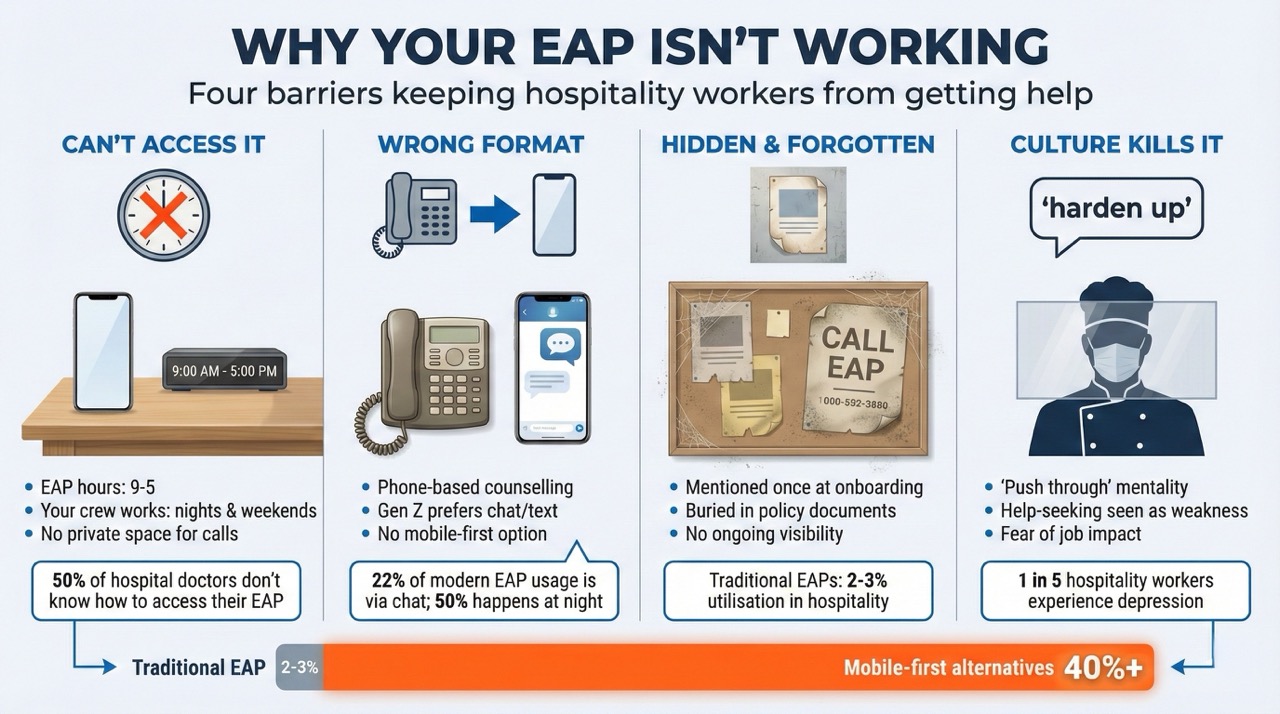
Problem 1: They can't access it
Traditional EAPs operate 9-5. Your crew works evenings, weekends, and split shifts. When they're struggling at 11pm after a brutal close, the EAP phone line is dark.
Even during business hours, where exactly is a kitchen hand supposed to take a confidential phone call? In the walk-in freezer? The break room where everyone can hear? There's no private space for the kind of conversation an EAP requires (PMC research; Sonder).
Many workers don't have personal laptops or reliable data plans. The technology assumptions built into traditional EAPs simply don't match frontline reality.
Problem 2: They don't know it exists
Here's a startling statistic: 50% of frontline hospital doctors – highly educated professionals in a healthcare setting – don't know how to access their EAP (Sonder).
If doctors can't figure it out, what chance does a 19-year-old casual with three weeks' tenure have?
EAPs are typically communicated once during onboarding, then buried in a policy document nobody reads. There's no ongoing visibility, no integration with daily work, no reminder that help exists when you need it.
Problem 3: The format is wrong
Traditional EAPs rely heavily on phone-based counselling. But Gen Z – who comprise the majority of your frontline workforce – find phone calls unfamiliar and uncomfortable.
The data is striking: 22% of Sonder's support cases come via chat, with 50% of usage occurring at night (Sonder BINGO Industries case study). Young workers want text-based, asynchronous support that fits their communication preferences.
A 2023 McKinsey study found 34% of Gen Z find digital mental health programs independently – they're actively seeking help, just not through the channels employers provide (McKinsey).
Problem 4: The culture kills it
Perhaps most damaging is what The Burnt Chef Project describes as the "banter, bollockings and beatings" culture normalised in commercial kitchens (ABC News, 2024).
In male-dominated kitchen environments, seeking mental health support is often viewed as weakness. The "harden up" mentality is explicit: 70% of food service workers face verbal or psychological abuse from customers, and reporting it or seeking help is seen as not being able to handle the job (Scratchie industry analysis).
Casual employment compounds this. When your shifts depend on staying in your manager's good graces, admitting you're struggling feels like career suicide.
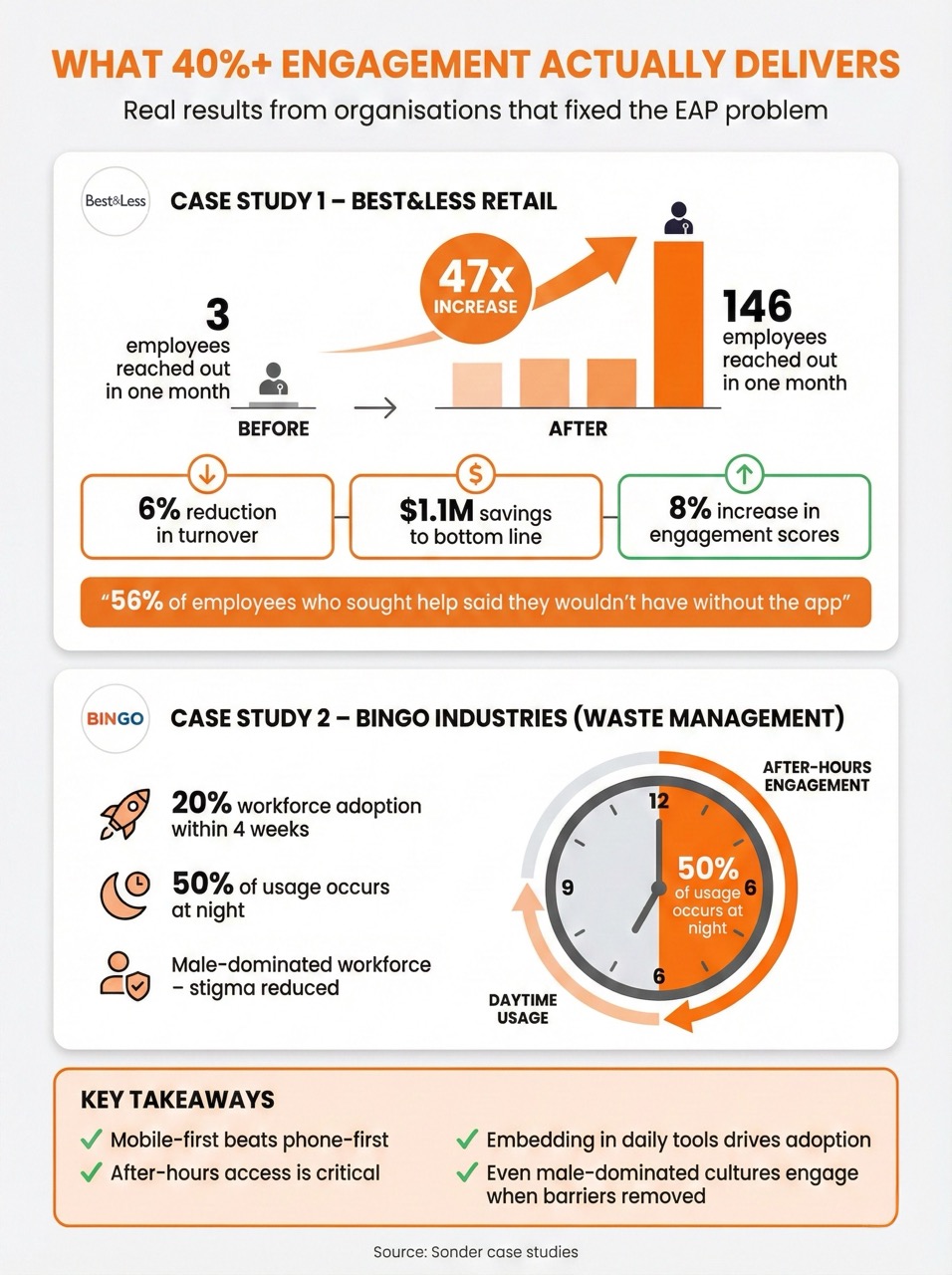
What Actually Works: The 40%+ Engagement Playbook
The contrast between traditional EAPs (2-3% utilisation) and modern alternatives (40%+ engagement) isn't marginal. It's transformational.
What's different?
Mobile-first, not phone-first
Modern platforms like Sonder deliver support through apps, not phone lines. Workers access help on the device they already carry, at times that suit them.
The BINGO Industries case study is instructive: within 4 weeks of launching Sonder, 20% of the workforce had engaged with the platform. 50% of app usage occurred at night – precisely when traditional EAPs are unavailable (Sonder case study).
At Woolworths Group, 56% of employees who sought help said they wouldn't have done so without Sonder's proactive, app-based approach (Sonder).
Proactive, not reactive
Traditional EAPs wait for workers to self-identify a problem and pick up the phone. That's a high bar when you're not sure if what you're experiencing "counts" as something worth calling about.
Modern platforms flip this. They push check-ins, surface resources proactively, and make it easy to engage before crisis hits. The shift from "call us when you're desperate" to "let's check in regularly" changes everything.
Integrated, not isolated
When mental health support lives in a separate app that workers have to download specifically for that purpose, most won't bother. The friction is too high for something that feels like admitting a problem.
But when wellbeing features are embedded in an app workers already use daily – for rostering, recognition, communication – the barrier disappears. Checking in on your mental health becomes as normal as checking your shifts.
Gamified, not clinical
Research shows gamification increases participation in wellbeing initiatives by 48% (TechReport survey; University of Colorado study). Elements like progress tracking, streaks, achievements, and friendly team competition transform engagement.
The "15 Minute Challenge" – a gamified workplace wellness program – achieved participation from 11,575 employees across 73 companies and demonstrated substantial health improvements (PMC research).
This isn't about trivialising mental health. It's about meeting people where they are, using mechanisms that actually drive behaviour.
The Business Case: What $1.1 Million in Savings Looks Like
Let's talk numbers that matter to operations.
Best&Less case study (Sonder):When the retail chain switched from a traditional EAP to Sonder's mobile-first platform, they saw 146 employees reach out for support in one month – compared to just 3 with their previous EAP.
The results:
- 6% reduction in turnover among employees engaging with the platform
- $1.1 million savings to the bottom line
- 8% increase in engagement scores, including "Organisational Fit" metric
Think about that turnover number in QSR terms. If you're running 20 stores with 50 crew each and annual turnover of 100%, even a 6% reduction saves you roughly 60 replacement cycles per year. At $5,864 per replacement (Cornell research), that's $350,000 annually – from a single intervention.
BINGO Industries case study (Sonder):In a male-dominated waste management workforce – a culture similar to many QSR environments – Sonder achieved:
- 20% workforce adoption within 4 weeks
- 50% of usage occurring after hours
- Measurable stigma reduction as workers who would never call an EAP started using the app
The common thread? Making support accessible, removing stigma through normalisation, and meeting workers in the digital environments they already inhabit.
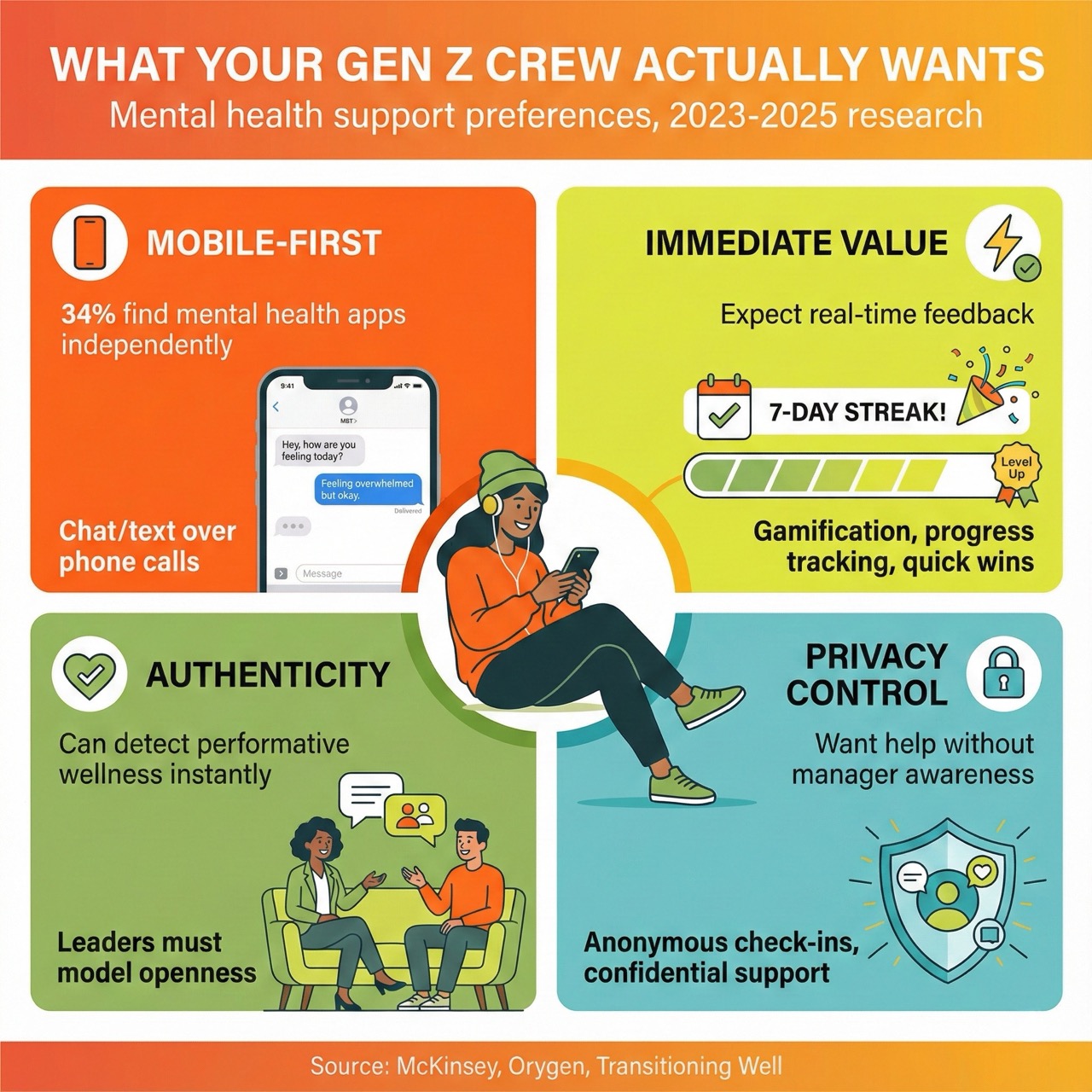
What Gen Z Actually Wants From Mental Health Support
Understanding Gen Z preferences isn't optional when they comprise the majority of your crew.
Research consistently shows this generation wants:
Authenticity over box-ticking
Gen Z can smell performative wellness from a kilometre away. They demand genuine, embedded wellbeing cultures – not a poster in the break room that nobody looks at (Transitioning Well; Executive Centre).
They want to see leadership model openness about mental health. When managers never acknowledge their own struggles, the implicit message is that admitting difficulty is unacceptable.
Digital-native experiences
34% of Gen Z find mental health apps independently (McKinsey). They're already seeking help – just not through the channels most employers provide.
They want chat and text over phone calls. They want mobile-first interfaces that work like the apps they use every day. They want privacy controls that let them seek help without manager awareness.
Immediate value, not delayed benefits
Gen Z expects instant feedback. Wellbeing tools that require weeks of engagement before showing any value will be abandoned immediately.
Gamification elements – progress tracking, streaks, achievements, quick wins – satisfy this expectation while building longer-term habits.
Holistic, not siloed
Young workers don't separate "mental health" from "safety" from "work satisfaction" the way corporate org charts do. They want integrated platforms that address their whole experience, not a different app for every category.
The Legal Reality: You Have a Duty Here
Since April 2022, Safe Work Australia's Model Code of Practice for managing psychosocial hazards at work has imposed explicit duties on employers (Safe Work Australia).
This isn't guidance. It's obligation.
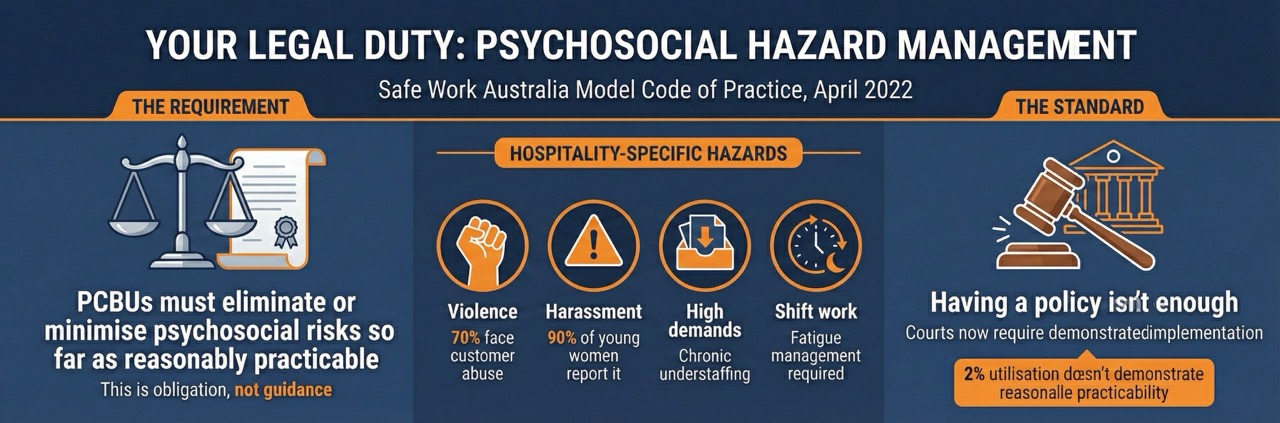
PCBUs must eliminate or minimise psychosocial risks so far as is reasonably practicable. They must consult with workers about psychosocial hazards. They must apply the hierarchy of controls to psychological risks – not just physical ones (Safe Work Australia; Pinsent Masons).
For hospitality specifically, this means documented prevention plans for:
- Workplace violence (70% of food service workers face customer aggression)
- Bullying and harassment (up to 90% of young female hospitality workers report sexual harassment)
- High job demands from chronic understaffing
- Shift work and fatigue impacts
Having a policy isn't enough. Recent court precedents have established that employers must follow their policies and demonstrate reasonable practicability. SafeWork NSW has successfully prosecuted employers for poorly handled workplace investigations – establishing that disciplinary processes themselves can constitute psychosocial hazards (Pinsent Masons).
The practical question isn't whether you have an EAP. It's whether you're actually meeting your duty of care when 97% of workers never use it.
Building Something That Actually Works
So what does effective mental health support look like in a QSR environment?
Embed it in something they already use
The number one predictor of whether workers will engage with wellbeing tools is whether those tools are already part of their daily routine.
If your crew uses an app for recognition, rostering, or communication, that's where mental health check-ins should live. Downloading a separate "wellness app" is friction most workers won't overcome.
Make check-ins rewarding, not mandatory
Mandatory mental health surveys create resistance and insincere responses. But optional check-ins with small rewards – points, recognition, entries into draws – transform participation.
Research shows 90% of employees say gamification boosts their productivity (Advantage Club; Psico-Smart). Apply the same mechanics to wellbeing and watch engagement multiply.
Use the data to intervene early
When check-ins are regular and participation is high, you get aggregated, anonymised data showing team-level trends. You can see when stress is spiking across a store, when particular shifts are struggling, when seasonal patterns emerge.
This lets you intervene before individuals reach crisis – adjusting rosters, adding resources, addressing specific issues – rather than waiting for workers' comp claims to tell you something went wrong.
Train managers to notice and respond
All the technology in the world won't help if frontline managers shut down conversations about mental health.
Black Dog Institute and Beyond Blue both offer workplace mental health training that builds manager capability to recognise warning signs, respond appropriately, and create psychologically safe environments. This isn't soft skill fluff – it's risk management.
Create pathways, not dead ends
Self-help tools and check-ins are valuable, but they're not treatment. Effective systems create clear pathways from low-intensity support (app-based resources, peer support) through to professional help (counselling, EAP services, clinical referral) when needed.
The goal is to catch people early, support them appropriately, and escalate when necessary – not to replace professional mental health care with gamification.
The Conversation Your Crew Can't Have (Until You Make It Possible)
Here's the thing about the "harden up" culture in hospitality: it doesn't mean workers aren't struggling. It means they're struggling silently.
When you create channels for anonymous check-ins, when you normalise conversations about mental health through visible engagement, when you remove the barriers that make traditional EAPs inaccessible – you're not creating problems that didn't exist.
You're finally seeing the problems that were always there.
One in three young hospitality workers experiences high or severe psychological distress (Healthy Workplaces SA). They're already in your stores, already on your rosters, already struggling. The only question is whether you know about it.
A 2% utilisation rate doesn't mean 98% of your crew is fine. It means 98% of your crew won't use the tools you've provided.
That's not their failure. That's yours.
The Bottom Line
Traditional EAPs were designed for a different workforce, in a different era, using different technology. Expecting them to work for young, mobile-first, shift-working hospitality employees is like expecting a fax machine to compete with WhatsApp.
The organisations seeing 40%+ engagement with mental health support aren't doing it through better EAP contracts. They're fundamentally rethinking how support is delivered:
- Mobile-first, not phone-first
- Embedded in daily tools, not isolated in separate apps
- Proactive check-ins, not reactive crisis lines
- Gamified engagement, not clinical presentations
- Normalised through regular use, not stigmatised through emergency-only framing
The business case is clear. The legal obligation is explicit. And the human case – reaching the 61% of your workforce experiencing mental health challenges – should be motivation enough.
The 2% problem isn't a mystery. The solutions are proven. The only question is whether you're willing to do something different.
Scratchie is developing Health Check features that embed mental health check-ins into the recognition app your crew already uses daily. Combined with ConvoCard for easy worker-to-manager communication, it's designed to reach the workers traditional EAPs never will. Email james@scratchie.com to learn more.
SOURCES REFERENCED
- Sonder – Average EAP Utilisation Rates (2-3% in hospitality)
- Healthy Workplaces SA – Hospitality Industry Profile (61% mental health conditions)
- Australian Bureau of Statistics – National Study of Mental Health and Wellbeing (21.5% general population, 38.8% for 16-24 year olds)
- Scratchie Industry Analysis – Mental health claims data (97% surge, $65,400 average cost)
- ABC News (March 2024) – Why Chefs Are Leaving the Hospitality Industry (Burnt Chef Project data, suicide research)
- PMC Research – EAP barriers for frontline workers
- Sonder – BINGO Industries Case Study (20% adoption in 4 weeks, 50% night usage)
- Sonder – Best&Less Case Study ($1.1M savings, 6% turnover reduction, 146 vs 3 contacts)
- Sonder – Woolworths Group data (56% wouldn't have sought help otherwise)
- McKinsey – Gen Z Mental Health: The Impact of Tech and Social Media (34% find digital programs independently)
- TechReport/University of Colorado – Gamification increases participation 48%
- PMC – 15 Minute Challenge study (11,575 participants, 73 companies)
- Advantage Club/Psico-Smart – 90% say gamification boosts productivity
- Safe Work Australia – Model Code of Practice: Managing Psychosocial Hazards at Work
- Pinsent Masons – Psychosocial Safety Obligations Analysis (court precedents)
- Transitioning Well – Gen Z at Work (authenticity expectations)
- Executive Centre – Workspace of Tomorrow (Gen Z preferences)
- Black Dog Institute – Workplace Mental Health Toolkit
- Beyond Blue – Workplace Mental Health Training Programs








.svg)
